
Simulation models
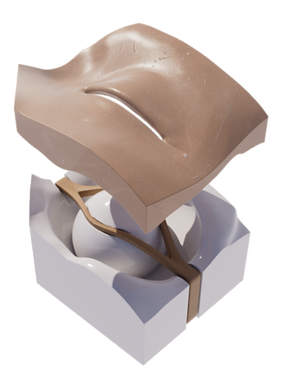
Certain skills, especially those involving manipulation of 3D structures, can be challenging to master with few opportunities for practice. We develop high-fidelity, cost-effective, and accessible models to simulate emergency procedures.
As a physician and medical illustration, I design simple, effective models to help clinicians practice essential procedures – especially in emergency and acute care settings.
These models are made to be affordable, anatomically accurate, and easy to use. Most are built around common procedures that benefit from hands-on repetition but are hard to teach on real patients.
Models and Use Cases
I’ve developed models for:
-
Lateral canthotomy
-
Foreign body removal
-
IV and intraosseous access (adult, pediatric, neonate)
-
Regional anesthesia (e.g., femoral, fascia iliaca blocks)
-
Flap design and suturing
-
Emergency airway landmarks and procedures
They’ve been used in residency workshops, procedure labs, and one-on-one teaching, often alongside brief didactic review and pre/post assessments.
Why I Build These
Many procedural skills are best learned through repetition, but access to realistic, low-cost models can be limited. I started making these models to fill gaps I saw in training and to make hands-on learning more accessible.
My background in anatomy and visual communication shapes how I approach model design, but the priority is always the learner: what they need to see, feel, and practice to build confidence and competence.
Design & Fabrication
Each model starts with a clinical question: What does the learner need to see, feel, or do in order to understand this procedure?
From there, I build outward using a combination of medical knowledge, anatomical references, and digital sculpting. Some models are shaped entirely by hand, while others are based on imaging data such as CT scans to ensure anatomical accuracy. I often simplify or exaggerate certain features intentionally to support procedural goals or highlight spatial relationships.
Once the design is finalized, molds are created and cast in silicone, sometimes layered over rigid cores to simulate bone or cartilage. Materials are chosen to balance realism with durability and cost so the models feel convincing in use, but are still practical for repeated teaching sessions. Many components are modular or replaceable, allowing for re-use across multiple learners or procedures.
Interested in Using or Adapting a Model?
I'm always happy to share ideas, collaborate on custom designs, or help integrate models into teaching sessions. If you’re looking to expand your procedural training tools, feel free to reach out.






